
For decades, MCB and the University of Illinois have been at the forefront of understanding the role of estrogen and the estrogen receptor (ER) in causing breast cancer. This is essential work: Breast cancer is the most commonly diagnosed cancer in women, affecting roughly one in eight women in the US alone.
MCB expertise began with the late Jack Gorski, co-discoverer of the estrogen receptor, the protein that estrogen must bind to in order to work. These days MCB faculty studying estrogen and ER include people like Milan Bagchi and Benita Katzenellenbogen, who have been here for a while, and others like Erik Nelson and Kannanganattu and Supriya Prasanth, who are relative new comers.
“MCB has been a major center for hormones and hormone action, especially as it relates to cancer, for many years,” says David Shapiro, inaugural Eugene E. Howe Scholar in Biochemistry. Plus, “we work well together, exchange ideas and technologies, and generally get along well.”
Enormous strides in fighting breast cancer have been made over the last few decades, with drugs that target estrogen production (aromatase inhibitors) and estrogen binding to ER, such as tamoxifen. Thanks in part to these drugs, breast cancer survival rates have improved.
However, although tumors often respond at first, cancer cells can mutate, become resistant and metastasize. Targeting these resistant tumors has become a high priority.
“This is the way of cancer,” says Shapiro. “It only very rarely can be eradicated with a single drug. The normal thing in cancer is that typically the tumors become resistant so you come up with different sequential treatments.”
Shapiro began his independent research career interested in the basic mechanism of how hormones work. As his work and the work of others began to illustrate how much hormones affected cancer cells, he shifted his focus to cancer. Like many others, Shapiro has lost close family members, including his mother, to cancer.
Cancer research is a crowded field. New tools are continually being developed and with these new tools, new understanding pushes the field forward. Shapiro has always been willing to seek out novel ways to look at and attack cancer. Recently that has involved screening tens of thousands of small molecules, not unlike looking for a needle in a haystack.
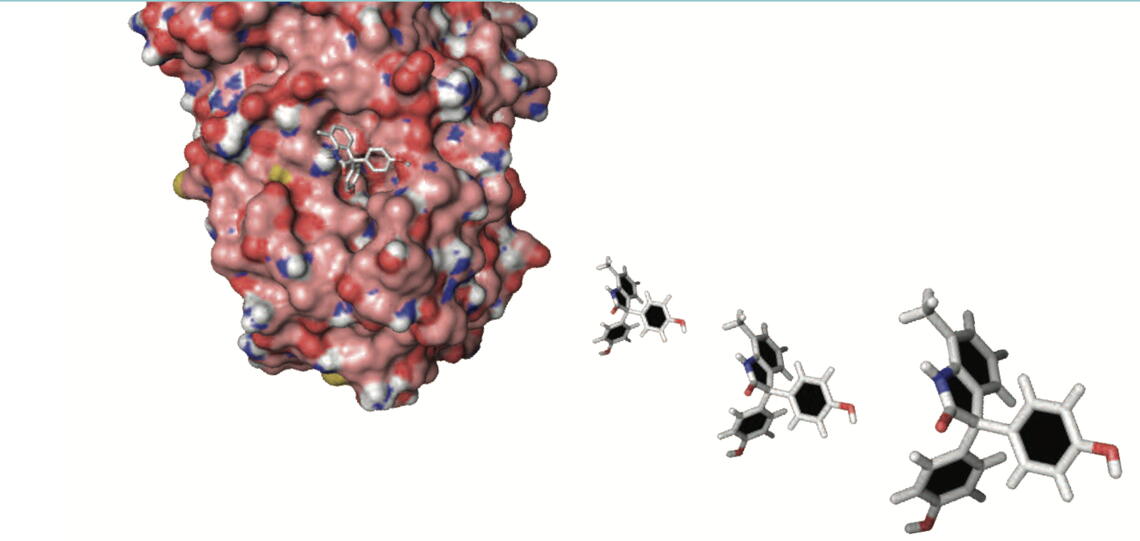
“About six years ago, I realized that there were 200,000 papers on estrogen and in order to discover something fundamentally different we’d have to try a new approach,” he says. With the help of colleagues experienced in using the high-throughput screening facility, Shapiro’s group screened 150,000 small molecules.
“Instead of looking at small molecules whose actions we could explain with current knowledge, we’d actually study the small molecules whose actions we could not explain, with a view to identifying entirely new ways estrogen works,” he says. “It turned out, happily for us, that the most effective molecule out of the 150,000 we screened worked in this exciting new way and led us to a normal pathway of estrogen action in cancer.That’s taken over most of our work.”
In other words, they found their needle. It is called BHPI.
In early experiments, BHPI appears to be highly effective, especially against drug- resistant cancers, precisely the cancers that are in Shapiro’s cross hairs.
BHPI was the only effective compound from the screen that works through the unfolded protein response (UPR) pathway. The UPR is a protective pathway and is turned on by stress, such as an unfolded or misfolded protein. Cancer cells use this same pathway to protect themselves from being killed by toxic anticancer drugs. If the protective pathway becomes overwhelmed, i.e. more unfolded proteins than it can handle, it revs up to a very high level, triggering a self- destruct process in the cells. Shapiro’s lab showed that estrogen bound to ER induces a moderate and protective activation of the UPR pathway in breast and ovarian cancer cells.
“BHPI hijacks this pathway and works through ER to throw the UPR pathway into overdrive, converting it from protective to lethal,” says Shapiro.
BHPI works even better in cancer cells resistant to anticancer drugs, because the UPR pathway is already turned on as part of the way cancer cells block the toxic action of anticancer drugs. This means that when BHPI turns the UPR up even more, those cells will tip over into the cell death pathway faster than in cells that are not under stress. Because the UPR is typically turned off in normal cells, when BHPI turns it on, it does not tip the UPR activation into the lethal range.This means healthy cells are not affected, says Shapiro.
BHPI also works by shutting down proteins that cells use to pump foreign compounds out of the cell. One way cancer cells become resistant to anticancer drugs is by using these pumps, called multidrug resistance proteins, to pump anticancer drugs out of the cells. Despite years of effort, drugs that directly block the action of the pumps have failed clinical trials. BHPI targets the multidrug resistance pump in a different way. One of BHPI’s actions is to open up a compartment within the cell that stores calcium.When the cell becomes flooded with calcium, protein pumps snap into action, pumping the calcium
back into the storage reservoir. But because the calcium continues to leak back into the body of the cell, the protein pumps burn through all the cells’ energy. Since the multidrug resistance pump also needs energy to work, it basically runs out of gas, sputtering to a stop.
Shapiro’s lab, in partnership with Nelson’s lab, used a mouse ovarian cancer model that is highly resistant to other drugs. They showed that not only did BHPI starve the multidrug resistance pump, it enabled the original drug to work again, since it was no longer getting pumped out of the cancer cells.
Yet another way cancer outwits anticancer drugs is by mutating the ER. One-third of metastatic breast cancers have mutated estrogen receptors; these changes are associated with resistance to drugs. So in another project, Shapiro used CRISPR gene- editing technology to replace the normal ER with each of the two most common mutations found in metastatic cancer. His team also tagged the cancer cells with the gene from fireflies that enables them to light up. Using state-of-the-art imaging equipment, this allowed the researchers to see, or image, the tumors inside the mice. In a small study, they found that BHPI was exceptionally effective.
BHPI and its cancer fighting potential is easily one of the most exciting findings in Shapiro’s long and successful career. The trick now is to continue down the road to clinical trials. Those efforts include collaborating with chemistry professor Paul Hergenrother, whose team is engineering new small molecules that might work even more effectively than BHPI. There are still many complicated and expensive steps ahead, but Shapiro is undaunted. Together with his colleagues, both in MCB and across campus, Shapiro will continue to match wits with cancer.
