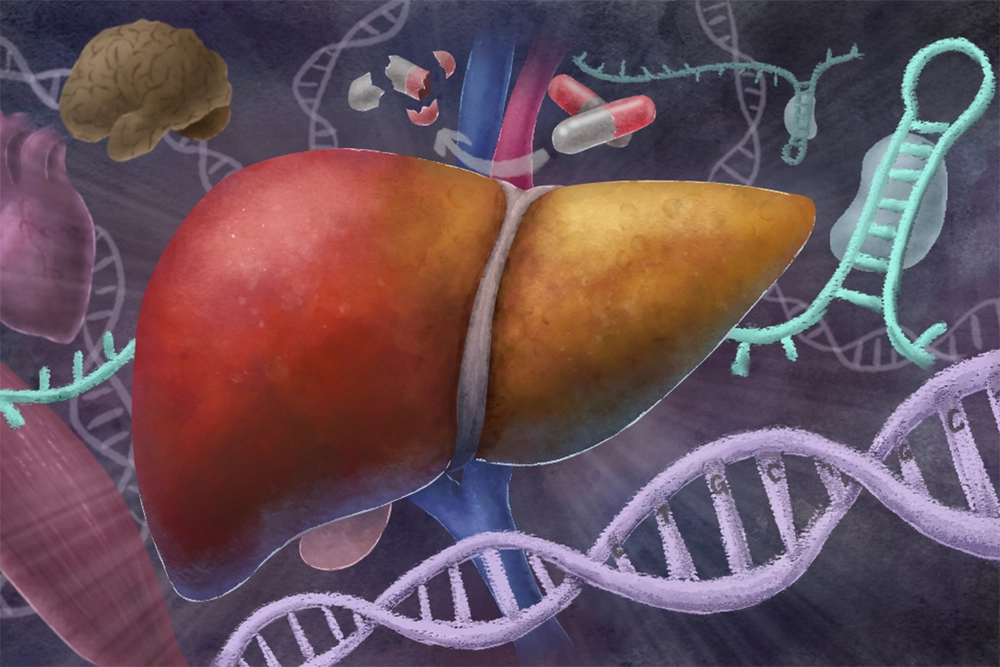
A new mouse model mimicking the liver symptoms of myotonic dystrophy type 1 — the most prevalent form of adult-onset muscular dystrophy — provides insight into why patients develop fatty liver disease and display hypersensitivity to medications, making treatment difficult. The new model opens avenues for screening new medications for liver toxicity prior to patient trials, University of Illinois Urbana-Champaign researchers said.
Led by U. of I. biochemistry professor Auinash Kalsotra, the researchers published their findings in the journal Nature Communications.
“This disease is not only a muscle disease; it’s a multisystemic disease. The mutated gene is in every cell,” Kalsotra said. “Most research has been focused on the muscle, or tying other symptoms to the muscle, and treatment development has been concerned with how to get therapeutics into the muscle. But most drugs go directly through the liver first. When new therapeutics for this disease go into trials, many show liver toxicity. So we need to understand what is happening in the liver.”
The disease is caused by a mutation in the DMPK gene. A three-letter sequence of CTG is repeated from dozens up to thousands of times. Although it is on a section that does not code for a protein, it is translated into toxic RNA that accumulates in cell nuclei. The repeating sequence causes the RNA to form tight hairpin loops, a structure that binds to and interferes with a class of RNA-binding proteins that regulate how other RNAs and proteins are spliced together.

Researchers have developed mouse models of the disease that produce the toxic RNA in their muscles, but none have ever targeted the liver, Kalsotra said. His team, led by graduate student Zachary Dewald, developed a line of mice that make the toxic RNA specifically in their liver cells. These mice displayed the same fatty liver symptoms and hypersensitivity to drugs often seen in human patients with myotonic dystrophy.
“It’s well known in the field of myotonic dystrophy that if a patient comes in for surgery, you cannot use regular anesthetics at regular dosages, because they may not wake up. But again, people thought that the sensitivity to these anesthetics and other drugs was being driven by the muscle tissue,” Kalsotra said. “Yet our mice, with the mutation only being expressed in liver cells and no other cell type, showed the sensitivity when we challenged them with various drugs. So we were very excited that by driving the disease in the liver, we now can see the liver effects on both the development of fatty liver and drug metabolism.”
While searching for the mechanism of why the toxic RNA results in fatty liver disease, the researchers found that a gene regulating fat synthesis, ACC-1, is misspliced and upregulated in the affected livers. They treated the mice with ACC-1 inhibitors and splicing correctors.
“We saw that just 10 days of treatment was able to reduce the lipid accumulation in these mice, showing us that the ACC-1 enzyme misregulation actually causes the fat accumulation we see in the disease — and that there are possible treatment pathways,” Kalsotra said.

To confirm that the effects they saw were only driven by the liver, rather than an interplay with muscle, the researchers compared their mice with another line of mice that express the mutated gene solely in muscle tissue. The researchers observed no issues with drug metabolism or fatty liver development.
“These findings really highlight the importance of studying the effects of myotonic dystrophy within individual tissues, and then evaluating their respective contributions to the metabolic dysfunction that is seen in these patients,” Kalsotra said. “We can’t just focus on one tissue type and completely ignore others.”
Kalsotra hopes for his group to next partner with clinicians to study biopsied liver tissues from human patients with myotonic dystrophy. If the pathology in human livers is confirmed to match that seen in the mouse model, the model could be useful for screening future therapeutics for toxicity and sensitivity.
“This will help us to ensure the effectiveness of prospective treatments that are being developed to treat this disease, as well as accordingly adjust dosages, keeping in mind that metabolism in the liver is altered for these patients,” Kalsotra said.
The National Institutes of Health, the Muscular Dystrophy Association, the Chan-Zuckerberg Biohub Chicago and the Beckman Fellowship from the Center for Advanced Study at the U. of I. supported this work. Co-authors included Dewald, Illinois postdoctoral researcher Haneui Bae, graduate students Oluwafolajimi Adesanya, Jessica Derham and Ullas Chembazhi, and undergraduate student Andrew Gupta.
Featured illustration by Haneui Bae.
The paper “Altered drug metabolism and increased susceptibility to fatty liver disease in a mouse model of myotonic dystrophy” is available online. DOI: 10.1038/s41467-024-53378-z
The National Institutes of Health supported this work through grants R01HL126845 and R01AA010154
Editor’s note: To reach Auinash Kalsotra, email kalsotra@illinois.edu. .